LipidMac: unveiling lipids role in tumor immunology
Diletta Di Mitri will lead the international consortium with the final aim of developing new immunotherapies to fight cancer
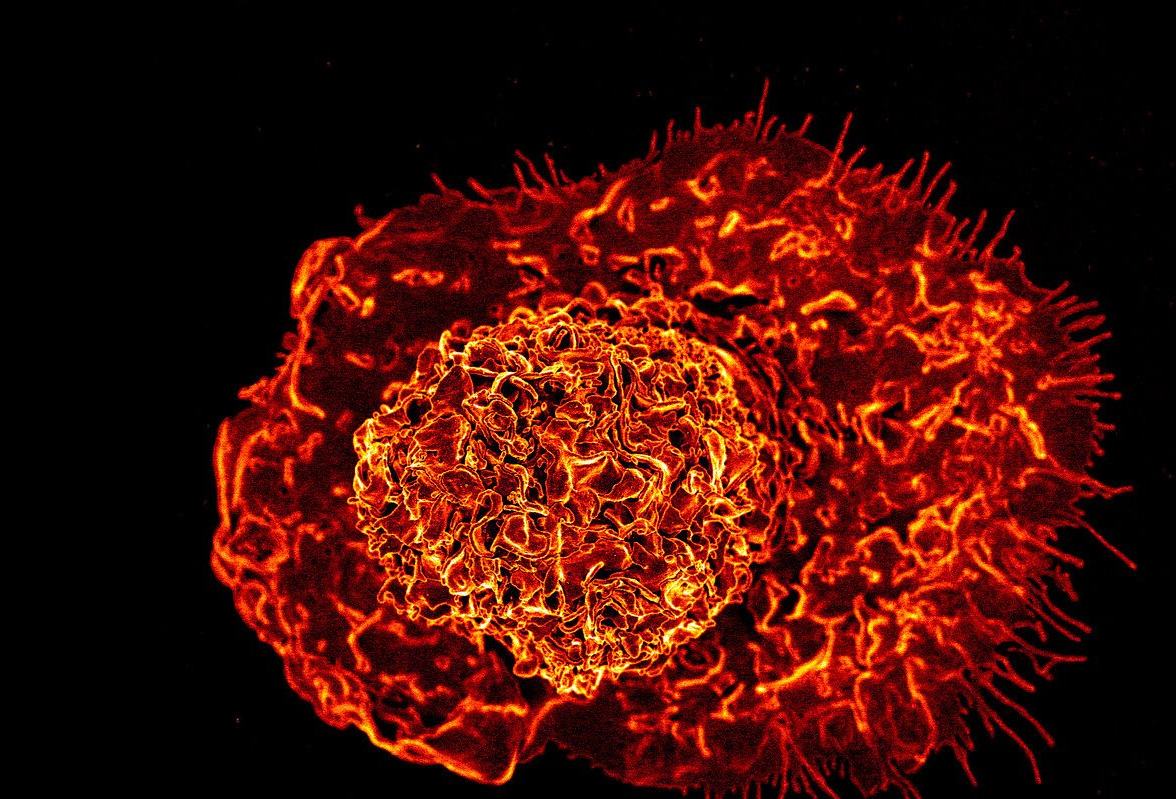
Almost all metabolic processes in cancer cells are accelerated: cancer cells consume more energy than healthy cells, accumulate more protein waste to be disposed of and, as known since a few years now, produce higher than normal quantities of fat molecules, the lipids.
But what is the role of these molecules? How do they affect the immune system’s ability to fight cancer? And what is the impact of high fat diets in fostering disease progression? These are some of the questions that LipidMac will try to answer.
The research project won the funds of the international Joint Translational Call 2021 dedicated to translational cancer research (TRANSCAN-3) and will start in January 2023. It brings together four international biomedical research institutions: Humanitas Research Hospital, Goodman Cancer Research Institute in Montreal, the National Center for Cancer Research in Madrid and the Gemelli Polyclinic in Rome.
The consortium will be coordinated by Diletta Di Mitri, head of the Tumor Microenvironment Lab at Humanitas Research Hospital and assistant professor at Humanitas University.
The study that inspired the LipidMac project
LipidMac will focus on three types of cancer – ovarian, breast and prostate cancer – and it is grounded in the results of a recent study conducted by Diletta Di Mitri’s research group and published in the Journal of Experimental Medicine (JEM).
As reported on JEM in December 2021, by studying prostate cancer, Humanitas researchers discovered that macrophages uptake fat molecules that are present in high quantities in the tumor microenvironment. By absorbing them, these lipid-loaded macrophages change their behavior, becoming precious allies for the tumor growth instead of hindering it.
Researchers have also discovered an antibody that is able – at least in the mouse model of the disease – to prevent macrophages from absorbing lipids. Its administration successfully slow down tumor growth and invasiveness, demonstrating the relevance of the mechanism as a possible therapeutic target.
“These promising results suggest new approaches for immunotherapy, different from those currently available – the so-called immune checkpoint inhibitors,” says Diletta Di Mitri. “But a lot of research still needs to be done. This is why been selected for TRANSCAN funding is so important: through the LipidMac project we will be able to better understand the role of lipids in tumors defense mechanisms and identify a shortlist of drug candidates capable of hindering their action and harnessing the anti-tumor activity of macrophages.”
LipidMac will also investigate – through a lab model – the effects of high-fat diets on disease progression. The hypothesis, already suggested by the previous study results, is that absorbing high percentages of fat through diet favors the availability of lipid molecules in the tumor microenvironment and therefore the presence of pro-tumor lipid-loaded macrophages.